A new report from the Centers for Disease Control and Prevention (CDC) has provided strong evidence that the HPV (human papillomavirus) vaccine is significantly reducing cervical cancer rates among U.S. women. The findings add to a growing body of research demonstrating the vaccine’s effectiveness in preventing one of the most common cancers affecting women.
The Role of HPV in Cervical Cancer
HPV is a widespread sexually transmitted infection (STI) and is the primary cause of cervical cancer. Certain strains of the virus, particularly HPV-16 and HPV-18, are responsible for nearly 70% of cervical cancer cases worldwide.
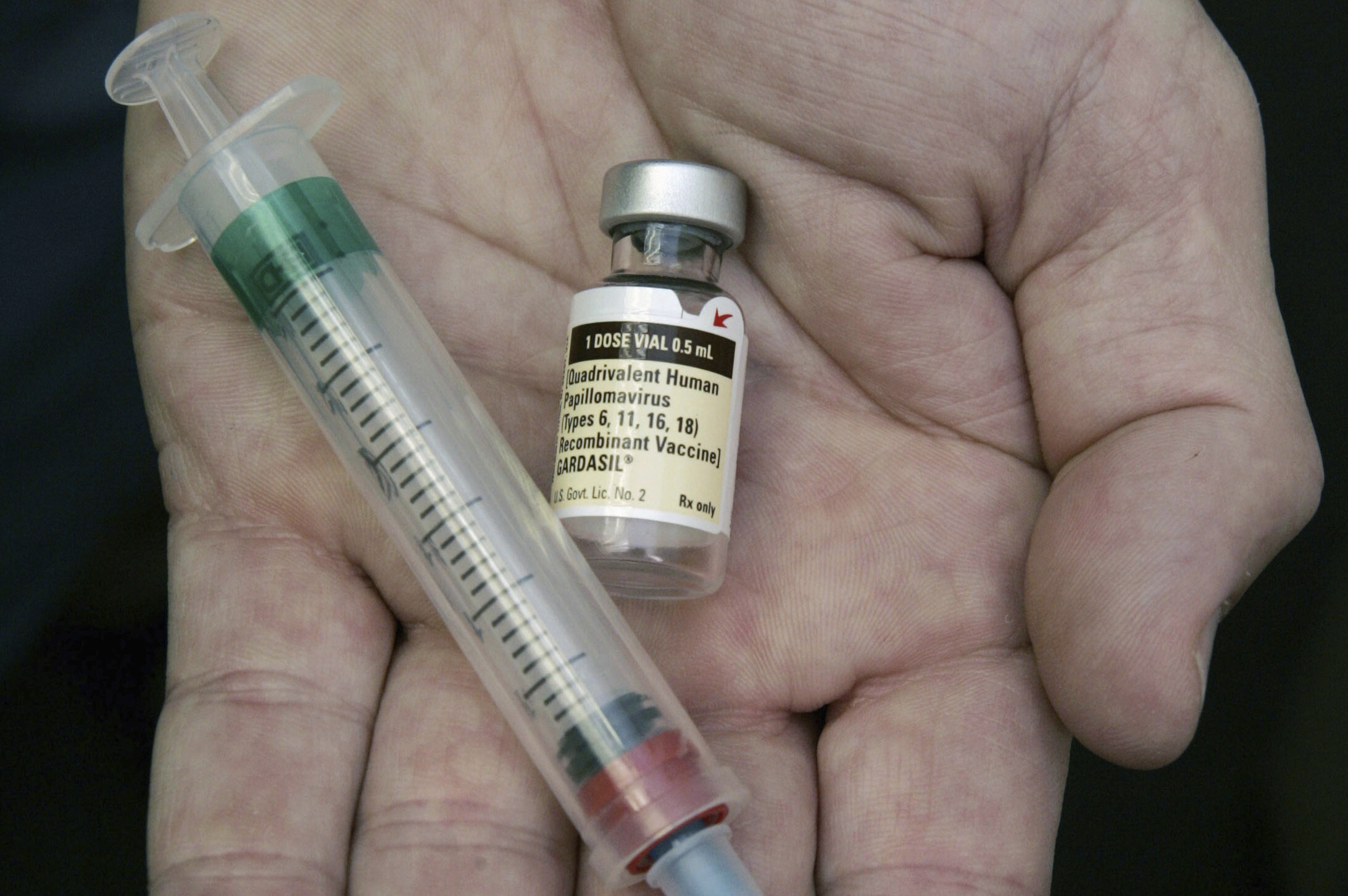
The HPV vaccine, first introduced in 2006, targets these high-risk strains, along with several others, preventing infections that could lead to cancerous cell changes in the cervix.
Key Findings from the CDC Report
The CDC’s latest research shows a significant decline in cervical cancer rates among vaccinated women. Some of the report’s key findings include:
- Sharp Decline in Precancerous Lesions: Women who received the vaccine, particularly those who were immunized before becoming sexually active, showed a notable reduction in precancerous cervical lesions.
- Decreased Cervical Cancer Rates: The incidence of cervical cancer has dropped, especially among younger age groups who were among the first to receive the vaccine.
- Herd Immunity Effect: Even among unvaccinated individuals, rates of HPV infections have declined due to reduced overall transmission in the population.
Challenges in Vaccine Uptake
Despite the vaccine’s proven effectiveness, vaccination rates in the U.S. still lag behind those of other developed countries. Some of the challenges include:
- Vaccine Hesitancy: Misinformation about vaccine safety and the belief that it promotes early sexual activity have led some parents to refuse the vaccine for their children.
- Access and Awareness Issues: Certain populations, particularly those in rural or low-income areas, have lower vaccination rates due to limited healthcare access.
Public Health Experts Advocate for Increased Vaccination
Medical professionals and health officials continue to stress the importance of increasing HPV vaccination rates. They recommend:
- Routine Vaccination: The CDC advises that children receive the HPV vaccine between ages 9 and 12 for maximum protection.
- Catch-Up Vaccination: Those who were not vaccinated at the recommended age can still receive the vaccine up to age 26, and in some cases, beyond that.
Conclusion
The CDC’s findings reinforce the HPV vaccine as a crucial tool in the fight against cervical cancer. While significant progress has been made, efforts to improve vaccination rates and awareness must continue to ensure that future generations are protected from this preventable disease.